How do we define success in a Medicare model such as Global and Professional Direct Contracting? Is it by the amount of money saved? Quality of care? Access to care? Expansion of populations served?
Such big-picture questions occupy minds at the Centers for Medicare & Medicaid Services (CMS) and other health care, government and financial leaders pursuing the holy grail of high-quality care at a reduced cost. They are particularly relevant to Direct Contracting, which aims to facilitate the shift from fee-for-service toward value-based care using capitated and partly capitated payments.
This voluntary risk-sharing model, which ended its first performance year December 31, has been in the news lately. Detractors’ criticisms have put additional pressure on CMS and its Center for Medicare and Medicaid Innovation (CMMI) to help their Direct Contracting Entities (DCEs) deliver on the model’s promise.
It has been “a growing year” for the DCEs, their partners in digital health and care coordination, and CMS, said David Ault, former CMMI senior advisor and division director. Ault shared his Direct Contracting insights during a recent webinar sponsored by naviHealth. In addition to providing an update on recent events, Ault pointed out issues that the federal agencies need to address and offered advice for those about to enter DCE engagements or considering doing so in 2023. He also laid out ways for providers to become successful DCEs.
2021: What we’ve learned
CMMI Deputy Administrator and Director Liz Fowler initially appeared ready to “put a pause on everything” related to Direct Contracting. Since then, however, her administration has come to “fully embrace” the model with some policy changes.
On the plus side of the ledger, CMS models are “somewhat iterative,” Ault said. “We have a seat at the table in working with CMS to design, develop and improve the models.” Direct Contracting “hiccups and hurdles” have included payment issues―providers receiving payments that should have been withheld under capitation rules, as well as providers not getting paid when they should have. While CMS is working to resolve these issues, there remains a gap in DCEs and providers knowing when the issues exist, creating headaches for doctors and the DCEs they work for.
In light of such issues, early and ongoing communication between DCEs and their providers is essential. DCEs must educate themselves and their partners on operational issues such as how to process capitated payments. It is also important for DCEs to let CMS know if the data gaps are creating problems for them. DCEs must also be sure that any providers joining the fold from other initiatives have given CMS timely notification of their termination in the previous program.
CMS is increasing the amount of real-time and other data and information it is providing. It’s also making clarifications in contracting terms, including a confirmation that provider agreements and fee reduction agreements can be at the entity level as opposed to the individual provider level. Also, DCEs will now be notified of retrospective adjustments quarterly rather than annually. These charges can still hit hard, but you won’t be blindsided at year’s end.
Another challenge for DCEs in 2021 was the amount of health care mergers, acquisitions, joint ventures and other major transactions. The lack of an application cycle in 2021 to start in 2022 “created a ‘taxi medallion’ system of DCEs trying to get in on other DCEs’ acceptances and trying to find creative ways to participate.” CMMI remains concerned about DCEs selling or transferring their ability to participate in the model. A DCE needs to look as similar as possible to what was in its application or what it looked like at its start. Having the same providers, beneficiaries and region will be very helpful.
Will 2022 be another transition year for Direct Contracting?
As CMS prepares for a new class of DCEs―the 2022 class will make it CMMI’s largest accountable care organization (ACO) model ever―it isn’t overly concerned about backlash on some fronts that Direct Contracting is a push to privatize Medicare. Those criticisms come primarily from a few progressive members of Congress and groups that see ACOs as a threat to their goal of Medicare for All, Ault said. Instead, CMS is focusing on determining what programmatic issues to address for 2023.
While there are new participation agreements for 2022, there are little to no significant policy changes.
“2022 is another transition year,” Ault said.“A year of ‘Let’s just keep the ship afloat, keep things going steady, let everybody keep getting up to speed before we get to bigger changes for 2023.’”
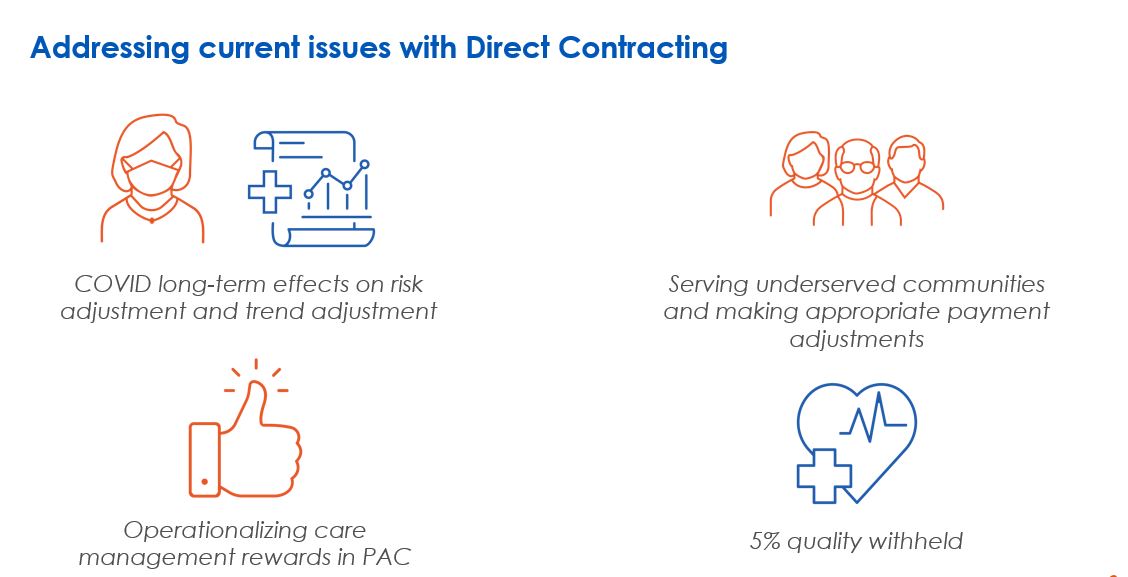
Questions remain about the pandemic’s effects on Direct Contracting, benchmarking, final settlements and how expenditures for COVID-19 episodes will be treated. As of now, CMS has not made any decisions and seems unlikely to do so before midyear. But it will be looking closely at risk and trend adjustment. “There needs to be input from everybody in this community on solutions,” Ault said. “The problem is that there’s not a good one-size-fits-all solution.” CMS wants to avoid allowing organizations to cherry-pick the options most favorable to them.
One notable programmatic change is the use of Consumer Assessment of Health care Providers and Systems (CAHPS) measures. This is just a “warmup” year, with CMS paying DCEs for reporting, not for performance. If you do it completely and report successfully, you get full credit. But in 2023, pay for actual performance on CAHPS scores will become a reality for standard and new-entry DCEs.
What needs to change beyond 2022
Pre-acute care: “I like to think about the pre-acute space and not the post-acute space,” Ault said. “If you’re out of the hospital, or in a SNF facility, or doing in-home post-discharge care―you’re automatically in that next pre-acute space. What can you do, not just in that week but in the next 30, 60, 90 days to provide appropriate care for that patient?” First, he said, the DCE team must pay attention to the discharge instructions and then combine resources and technology across transitions of care.

High-level changes: This year is when Ault expects to see some major changes, starting with an announcement in late March or early April previewing the model for 2023 forward. Former CMS Administrator Donald Berwick and former CMMI Director Richard Gilfillan have raised issues about the sustainability of high performance by ACOs. Ault expects some high-level benchmarking changes, possibly including a “reweighting” of historical expenditures, a “change in the regional blend,” or tweaks to certain discounts and exemptions. The 5% quality withhold is likely to be reduced or otherwise adjusted.
Time to express concerns: At this point, Ault said, there’s still time for you to reach out to CMS to express any concerns you might have, though the model will continue. “I fully expect that there’s going to be another application cycle for 2023, and then all these concerns about changing control and ‘taxi medallions’ will go away, and everybody will have a chance to apply and participate,” he said. He expects the next class to be smaller than the current one, more like 15 to 20.
Diversity and health equity: With diversity and health equity a focus of the Fowler administration, the 2023 model could include favorable benchmarking, an upfront funding mechanism or other incentives to encourage DCEs to enter underserved communities.
Pain points create opportunity: Pain points for patients and providers include patient difficulties post-discharge, identifying appropriate care settings and patient access, and hospital “frequent flyers.” These challenges create an opportunity to improve care and change future behavior.
Click below to watch the naviHealth webinar “Direct Contracting changes are coming: What to note for 2022 and beyond” featuring former CMMI Senior Advisor and Division Director David Ault.