Alternative payment models (APMs) are on many people’s minds these days as the new players in the Biden administration begin to focus on the path toward value-based care.
On July 1, the Centers for Medicare & Medicaid Services (CMS) unveiled the modified end-stage renal disease (ESRD) payment model, its first value-based payment model directly addressing health equity. This could mark the Biden administration’s first steps in the shift to value-based care, after it had put numerous rules on hold or under evaluation. The value-based ESRD program and direct contracting are two of the latest pieces of the puzzle amid the industry’s move toward value through the use of APMs. Industry observers are predicting a mandatory APM by the end of January.
In the meantime, let’s take stock of where we stand with APMs in general—and in particular with direct contracting, a set of voluntary payment model options aimed at, in CMS’ words, “reducing expenditures and preserving or enhancing quality of care for beneficiaries in Medicare fee-for-service (FFS).”
ESRD model seeks to reduce disparities
The value-based payment model presented by the Biden administration would give dialysis providers incentives to reduce disparities in home dialysis and kidney transplant rates among patients from disadvantaged areas, Healthcare Dive reported. It would modify the existing ESRD Treatment Choices Model’s benchmarking and scoring methodology in the effort.
The proposed rule would update the ESRD Prospective Payment System for calendar year 2022.

ESRD disproportionately affects disadvantaged Medicare patients, who tend to have higher hospital readmissions and costs, CMS research has found. In addition, Healthcare Dive has reported that ESRD patients from various racial and ethnic backgrounds “are less likely to receive pre-ESRD kidney care, be waitlisted for a transplant or get a new kidney.”
Liz Fowler, who assumed leadership of the Center for Medicare & Medicaid Innovation (CMMI) this year, has demonstrated a commitment to health equity for rural and urban communities, while also stressing sustainability. One of her priorities will be to oversee the creation of APMs that, once the test stage has passed and CMS funding has been exhausted, can survive and succeed on their own.
“Disparities in … access to care have plagued our health care system and negatively impacted populations of color for as long as we’ve had a health care system,” Fowler told Health Affairs editor in chief Alan Weil during a June 3 appearance on C-SPAN’s Health Affairs Speaker Series. “But COVID has exposed inequities that are impossible to ignore and brought the issue into the mainstream. And with this increased visibility, health care stakeholders and policymakers are charging forward with solutions.”
CMS replaces Next Generation ACOs with direct contracting
CMS will not extend or expand the Next Generation ACO (NGACO) Model, it announced May 21. That program, which took effect January 1, 2016, and previously received a one-year extension because of COVID-19, is set to end December 31. In its place, CMS introduced the Global and Professional Direct Contracting (GPDC) Model test.
The GPDC Model got underway April 1 with 53 “direct contracting entities (DCEs),” according to a report in Home Health Care News. That publication described direct contracting as “one of the newest alternative payment arrangements from CMS and its innovation hub,” adding: “Broadly, direct contracting with CMS gives private health care providers a chance to engage in risk-sharing arrangements with traditional Medicare, hoping the concept brings down costs and improves care. There are various direct-contracting ‘options,’ with each side presenting a different level of potential upside or downside risk.”
NGACOs had until June 14 to request to join the GPDC Model, which CMS has characterized as a high-risk financial arrangement and APM mechanism similar to its predecessor. CMS said the model could leverage NGACOs’ operational capacity and processes―built over the course of the model’s life―to do value-based health care transformation work.
Direct contracting, which involves a per beneficiary, per month payment to a health care organization to cover most of the care for a given plan member, is considered a value-based care arrangement in Medicare FFS. One health care executive told Home Health Care News that he had “been really surprised by the bipartisan support for direct contracting.”
Different levers for success

Faegre Drinker counsel
During a webinar with naviHealth, Faegre Drinker counsel David Ault described the direct contracting model as a new fee-for-service opportunity with different levers for success. According to Ault, these APMs are unique in its combination of financial risk (expenditures and quality) and capitation, with success depending on appropriately managing pre- and post-acute care through two participation tracks: a Professional Option with share savings/losses of 50%, and a Global Option with shared savings/losses of 100%.
“There are levers in place in this model that haven’t been in place before,” said Ault, who advises health care providers and payers on the regulatory, compliance and litigation aspects of health insurance. “Specifically it is balancing capitation with risk. So you can be at the full risk, but you now have this upfront capitation, which gives you an opportunity to engage with providers and beneficiaries in a way that you never had before.”
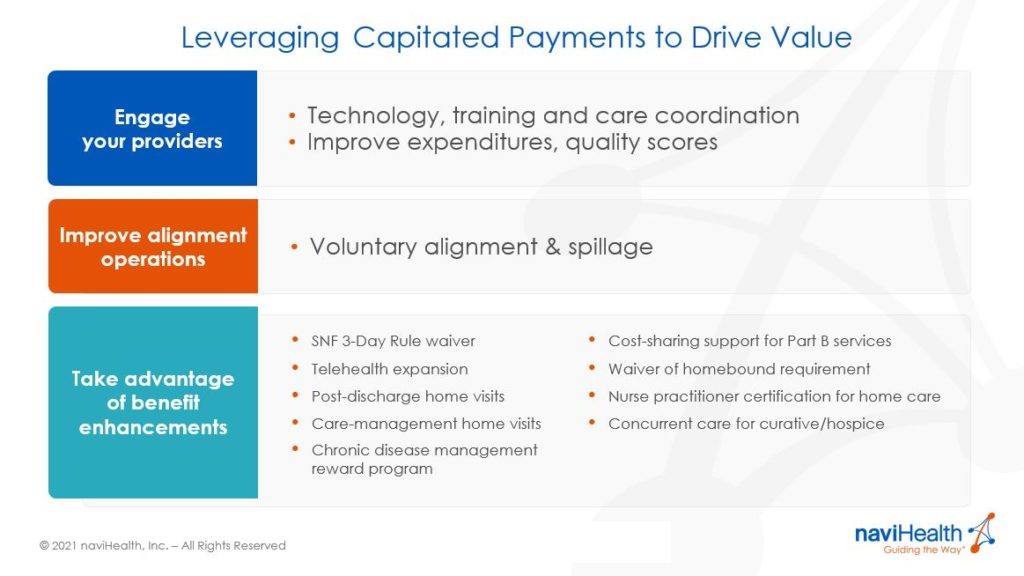
Appropriately managing the pre-acute space, Ault said, means “keeping beneficiaries healthy ― those who are at highest risk, those with multiple chronic conditions, comorbidities ― really engaging with them to keep them from having an acute event.” As for post-acute patients, it means “finding the proper care for them, meeting the patient where they are, getting them in the appropriate setting and keeping them there for the appropriate time.” Success in those areas, he said, will keep expenditures down and help organizations succeed on the all-important quality measures.
By leveraging capitated payments to drive value, Ault said, health care organizations can engage providers, improve alignment operations and take advantage of benefit enhancements such as care-management home visits, chronic disease management reward programs and the recent expansion of telehealth benefits.
Interested in learning more about Direct Contracting and other APMs? Click here to watch the naviHealth on-demand webinar featuring David Ault.